If you’ve been managing your blood pressure, you’re probably well aware of its high’s and low’s.
You delight in a low blood pressure, but when your diastolic pressure (represented by the bottom number in your blood pressure reading) is low, you may be at risk for the following:
- New-onset heart failure
- Brain atrophy
- Increased mortality if you have chronic kidney disease
 Diastolic blood pressure measures the pressure within your arteries as it flows through them. It’s the pressure between heartbeats, that is, when your heart is at rest.
Diastolic blood pressure measures the pressure within your arteries as it flows through them. It’s the pressure between heartbeats, that is, when your heart is at rest.
Systolic blood pressure (represented by the top number in your blood pressure reading) measures the amount of pressure that your blood exerts on vessels when your heart contracts or ‘beats’.
Isolated Diastolic Hypotension
“Isolated diastolic hypotension” (IDH) is a condition that occurs when your diastolic blood pressure is low (less than 60 mm Hg), but your systolic blood pressure is 100 mm Hg and above.
If you’ve been congratulated for having a good systolic blood pressure (less than 120 mm Hg — or even less than 130 mm Hg), don’t be so quick to start your celebratory dance. What’s your diastolic blood pressure? Many clinicians don’t consider a low diastolic blood pressure reading as problematic.
New-Onset Heart Failure
According to a study, older adults with low diastolic blood pressure have an increased risk for developing new-onset heart failure and a higher risk of death. The researchers studied nearly 2,400 Medicare-eligible adults who were 65 years and older and followed them for over 12 years.
If you have a low diastolic blood pressure but an elevated systolic blood pressure, it can be challenging for your physician to treat.
The Right Dose
 Finding the appropriate dose of anti-hypertensive medication is a dilemma. You need a high enough dose to lower the systolic pressure to normal levels without reducing the diastolic pressure to below 60 mm Hg.
Finding the appropriate dose of anti-hypertensive medication is a dilemma. You need a high enough dose to lower the systolic pressure to normal levels without reducing the diastolic pressure to below 60 mm Hg.
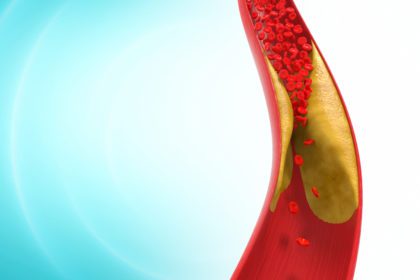
Patients with hypertension, coronary artery disease AND low diastolic blood pressure have been shown to have poor outcomes.
Based on the findings of this study, intensive lowering of systolic blood pressure with medication in these patients could result in excessive reduction in diastolic blood pressure — and should be avoided.
Per the results of this study, diastolic blood pressure should be kept at 60 mm Hg and higher in older adults. It was suggested that future hypertension guidelines should focus on optimal diastolic blood pressure parameters for older adults on anti-hypertensive medication.
Brain Atrophy: A Sign of Early Vascular Aging
In a study of patients diagnosed with coronary artery disease (not cerebrovascular or peripheral artery disease), there appears to be a link between brain atrophy (shrinkage) and low diastolic blood pressure.
A baseline diastolic blood pressure of 70 mm Hg or less showed a significantly higher rate of atrophy in various regions of the brain.
Although reducing blood pressure is generally beneficial, the researchers concluded that lowering blood pressure with anti-hypertensive medications can be overdone.
If diastolic blood pressure is already on the low end, based on these findings, further treatment should be approached with caution. Here’s how the researchers explained the possibilities for their findings:
- Reduced blood pressure results in reduced cardiac output. This means less blood is flowing to the brain resulting in accelerated brain atrophy.
- Brain atrophy may actually cause low blood pressure.
- Impaired cerebral autoregulation – a specific mechanism makes the brain more vulnerable to lower blood pressure levels.
NOTE: Other research has revealed that the brain shrinks a decade before the symptoms of Alzheimer’s disease appear.
Chronic Kidney Disease and Blood Pressure
Added to the list of conditions that appear to be adversely affected by low diastolic blood pressure is chronic kidney disease (CKD).
An observational study suggests that the aggressive use of anti-hypertensive medications to lower systolic blood pressure — which also lower diastolic blood pressure to less than 70 mm Hg — may increase mortality risk for patients with chronic kidney disease.
In this study, nearly 652,000 male U.S. veterans (mostly white males averaging 74 years old) with chronic kidney disease were followed for approximately six years.
The researchers found that kidney disease participants with a systolic pressure of less than 130 mm Hg and a diastolic pressure of less than 70 mm Hg had a higher risk of death.
Trying to achieve ideal systolic blood pressure could place patients with CKD at risk if it causes their diastolic pressure to go below 70 mm Hg. They found that the optimal blood pressure for patients with CKD is:
- Systolic pressure of 130 to 159 mm Hg (Stage 1 hypertension) AND
- Diastolic pressure of 70 to 89 mm Hg
IMPORTANT! Be sure that your blood pressure readings are accurate and not “artificially” high. See How to Avoid Artificially High Blood Pressures.
Since a low diastolic blood pressure is an independent risk factor for several medical conditions, you must be certain that you’re not started on anti-hypertensive medication unnecessarily or that your prescribed dosage is not too high to cause your diastolic pressure to go below 70 mm Hg.
![]() Karen’s Fit Tip: Take aggressive control over your own cardiovascular risk factors. Work on reducing your blood pressure by following a healthy eating plan and regular exercise routine, stopping smoking, managing your stress and blood sugar, and committing to losing weight.
Karen’s Fit Tip: Take aggressive control over your own cardiovascular risk factors. Work on reducing your blood pressure by following a healthy eating plan and regular exercise routine, stopping smoking, managing your stress and blood sugar, and committing to losing weight.
 If you’re on anti-hypertensive medication, be sure you track your own blood pressures at home with a reliable home blood pressure monitor.
If you’re on anti-hypertensive medication, be sure you track your own blood pressures at home with a reliable home blood pressure monitor.
Keep a log of your blood pressures to show your physician. Download the attached daily blood pressure log form and blood pressure checklist: blood-pressure-log.
Make sure you are using the right size blood pressure cuff and know the factors that affect your blood pressure readings. Know them. Memorize them.