To limit the global spread of COVID-19 and to “flatten the curve”, the advice to stay at home has presented one particular group with a unique set of challenges. That group is people with arthritic diseases, especially those with osteoarthritis. Osteoarthritis affects twenty percent of Americans and eighty percent of people older than age 55. Our health expert, Karen Owoc, is here to tell us more about this condition and the best way to manage the symptoms during a COVID-19 era.
What is Osteoarthritis?
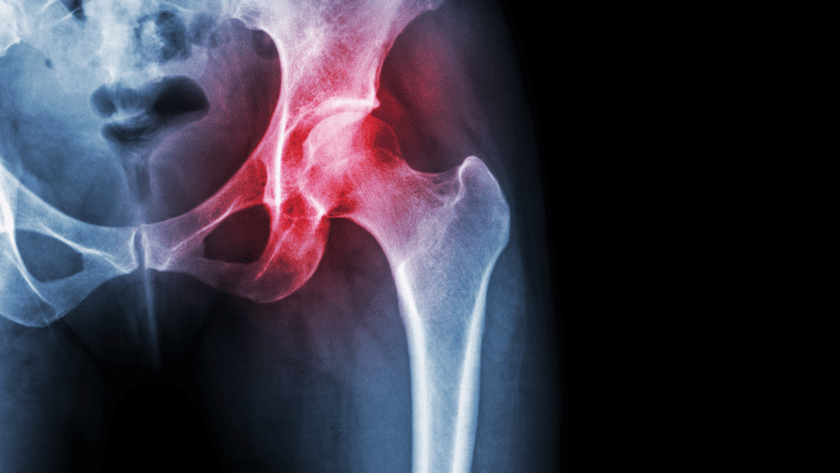
Osteoarthritis (OA) is known as “wear and tear arthritis” vs. rheumatoid arthritis (RA) which is an autoimmune, inflammatory disease. An autoimmune disease means your immune system attacks healthy cells in your body by mistake, which results in painful swelling (inflammation) in the areas that are affected. Typically RA attacks multiple joints.
Joints are places in the body where bones meet. Joints are different shapes, sizes, and allow you to move. They roll, glide, rotate, and bend. All joints are susceptible to wear and tear, damage, and arthritis — particular joints in the hand, hip and knee.
Osteoarthritis and COVID-19
OA is the most common degenerative disease of the joint and impairs quality of life and leads to significant disability. There is no documented increased risk of respiratory infections for OA patients compared with the general population. Inflammation, biomechanical stress, and immune response play an important role in initiating the disease.
OA patients have an increased risk of death during infections due to the presence of associated disorders. Osteoarthritis patients often show a large array of other underlying medical conditions, which are shared with COVID-19 patients and may therefore increase life-threatening COVID-19 complications (the overreactive immune response).
- Diabetes
- Inflammation
- Cardiovascular disease
- Hypertension
- Low muscle mass
- Obesity
OA patients living in severe pain and disability had been unable to have joint replacement surgeries because they were considered an “elective surgeries”. Until recently, they were also unable to receive pain-relieving joint injection treatments (cortisone) and supplements) when visits to doctors’ offices were limited to medical emergencies.
Who’s at Risk for Osteoarthritis
- Over at 50
- Post-menopausal women
- History of joint injury (e.g., athletes)
- Obesity
Management of OA During the COVID-19 Era
The most recent (2019) guidelines per the American College of Rheumatology and Arthritis Foundation for management of hand, hip, and knee osteoarthritis (especially those who are overweight or obese) is exercise and weight loss.
Since the only hope of managing OA symptoms is exercise and weight management, recommendations for core treatment are to exercise as often as possible — regardless of age, other conditions, pain severity or disability. However, the closure of gyms, swimming pools and parks, and limited use of open spaces to promote social distancing means that OA patients must keep moving and exercise at home (or close to home) and eat a healthy diet.
Tips to Minimize Joint Deterioration (Habits for Healthy Joints)
Protect joints to maximize their use, mobility, function, and longevity.
- Build muscle. Very strong joints need muscles. They surround joints and support, stabilize, and guide joints through range of motion (ROM). Strength improves balance and reduces risk of sustaining trauma to joints in a fall.
- Stretch every day. Manipulate all the body parts through full ROM that you plan on using the rest of your life (e.g., fingers, wrists, arms, anchors, shoulders).
- Do balance exercises, Tai chi, Pilates, and yoga. This type of physical training helps improve joint function and proprioception in osteoarthritis patients. Chair-based variations are also recommended.
4. Don’t jump. Jumping adds joint load of 20X your body weight.
Coming up next... Stay tuned for more tips in Part 2 on this topic!
![]() Karen’s Fit Tip: Keep moving to manage osteoarthritis symptoms. Take advantage of online modified exercise classes and videos. Consult a professional therapist or clinical fitness specialist and follow an anti-inflammatory diet.
Karen’s Fit Tip: Keep moving to manage osteoarthritis symptoms. Take advantage of online modified exercise classes and videos. Consult a professional therapist or clinical fitness specialist and follow an anti-inflammatory diet.