According to the Centers for Disease Control and Prevention, more men die from cancer, heart disease, injuries, stroke, and diabetes than women, but… they’re half as likely to go to the doctor for annual exams and preventive care. Preventive care saves lives as many diseases that kill men are SILENT.
The Silent Killers of Men
Silent Killer #1: Abdominal Aortic Aneurysm (age 65+)
If you are between the ages of 65 and 75 and have ever smoked, i.e., 100 or more cigarettes during your lifetime, you should be screened once for an abdominal aortic aneurysm (AAA).
 AAA is very common with over 3 million Americans afflicted every year. This type of aneurysm, “The Silent Killer”, is an abnormally large or swollen blood vessel in your abdomen. It is diagnosed by abdominal ultrasound, MRI, or CT scan.
AAA is very common with over 3 million Americans afflicted every year. This type of aneurysm, “The Silent Killer”, is an abnormally large or swollen blood vessel in your abdomen. It is diagnosed by abdominal ultrasound, MRI, or CT scan.
Aneurysms may tear or rupture if left untreated and cause massive internal bleeding. Ruptures are very painful events and may result in permanent disability or death. Their exact cause is unknown, but risk factors for developing an abdominal aortic aneurysm (AAA) include:
- Advanced age
- Emphysema
- Genetic factors
- High blood pressure
- High cholesterol
- Obesity
- Male gender
- History of smoking
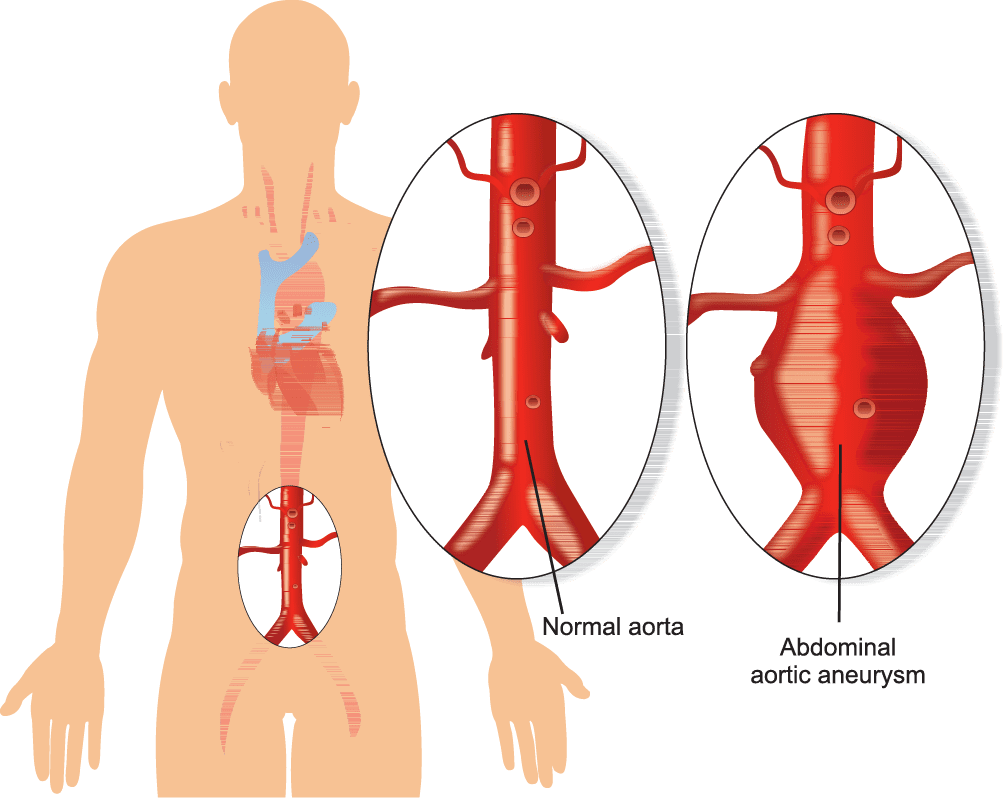
The aneurysm bulges outwardly, like a bubble or balloon. Caused by a localized, abnormal, weak spot on a blood vessel wall. The result of a WEAKENED blood vessel wall.
Silent Killer #2: Prostate Cancer (screen at age 50+ or earlier depending on risk)
According to the Centers for Disease Control and Prevention, approximately 39 out of 100 men in the U.S. will develop cancer during their lifetime. 80% of all cancers in the United States are diagnosed in people 55 years of age or older.
Next to skin cancer, prostate cancer is the most common type of cancer found in American men. Prostate cancer is the second leading cause of cancer death in men. About 1 man in 41 will die of prostate cancer. (Lung cancer is first.)
When to screen for prostate cancer:
- Age 50 for average-risk men
- Age 45 for men at high risk – African-Americans
- Age 40 for men with a strong family history of prostate cancer
Screening involves a yearly prostate-specific antigen (PSA) blood test and digital rectal exam (DRE) for men beginning at age 50 with at least a 10-year life expectancy. Watch the interview below about prostate cancer/robotic surgery with Dr. Neil Okamura and Dr. Mark Lollar…
Credits: John Kessler, former Co-Anchor for the KPIX CBS 5 Eyewitness News Early Edition and Emmy Award recipient.
In comparison to breast cancer in women:
- Nearly 30% more men are diagnosed with prostate cancer (157 men per 100,000).
- Over 4% more men died from prostate cancer (25 men per 100,000).
However, “years of life lost” is greater in breast cancer since men typically die of prostate cancer at an older age than women die of breast cancer.
Based on these statistics*, breast cancer appears to be more destructive despite there are more deaths from prostate cancer.
*Using official data, researchers in England estimated the years of life lost, for both cancers. This involved estimating how many people died of each disease at each age group, then subtracting that number from the life expectancy in England (around 80 years old).
Government guidelines recommend AGAINST a routine PSA for prostate cancer due to the screening benefits and harms (e.g., false positives, false negatives, “overdiagnosis”, and “overtreatment”).
However, the American Cancer Society recommends discussing the limitations and potential benefits of prostate cancer early detection testing and should include the offer to test.
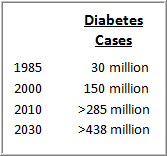 Silent Killer #3: Type 2 Diabetes (screen at age 45+ or according to risk)
Silent Killer #3: Type 2 Diabetes (screen at age 45+ or according to risk)
- 1 in 3 Americans has diabetes and/or pre-diabetes.
- 1 in 10 Americans (9.4%) has type 2 diabetes.
- 90% with pre-diabestes don’t know they have it.
Uncontrolled diabetes, a lifestyle disease, can lead to:
- Heart disease (leading cause of death in the U.S.)
- Stroke
- Kidney disease
- Blindness from damage to blood vessels in the eye
- Nerve damage (extremities which can lead to amputation, loss of feeling, resulting in fall risk)
- Impotence (blood vessel damage)
Starting at age 45, screen for type 2 diabetes (a blood test). Test earlier if you have any of the following risk factors as they can increase your risk of getting this disease:
- Family history of diabetes
- Race or ethnic background – Hispanics, Blacks, Native Americans, and Asians tend to be more highly affected.
- Metabolic syndrome (also called insulin resistance syndrome)
- Overweight – Defined as a Body Mass Index (BMI) greater than 25.
- Habitually inactive
- Hypertension (high blood pressure)
- Abnormal cholesterol levels – HDL (“good”) cholesterol level is under 35 mg/dL (milligrams per deciliter) and/or triglyceride level is over 250 mg/dL.
- History of vascular disease (such as stroke)
Silent Killer #4: Colorectal Cancer (screen at age 50; age 45 for African-Americans)
Colorectal cancer is the third leading cancer killer in men. Colon cancer is often diagnosed at a very late stage because of its lack of symptoms – which is why it is often referred to as a “silent killer”.
Starting at age 50, your physician can decide which test is right for you (e.g., sigmoidoscopy, colonoscopy, CT scan, barium enema). Occasional bowel changes are normal. Listen closely to what your body is telling you. Bowel changes may be early symptoms of colon or rectal cancer, especially if they come on suddenly.
Diagnosing colon cancer at Stage 0, 1, or 2 versus Stage 3 or 4 can be the difference between living and dying. Get screened.
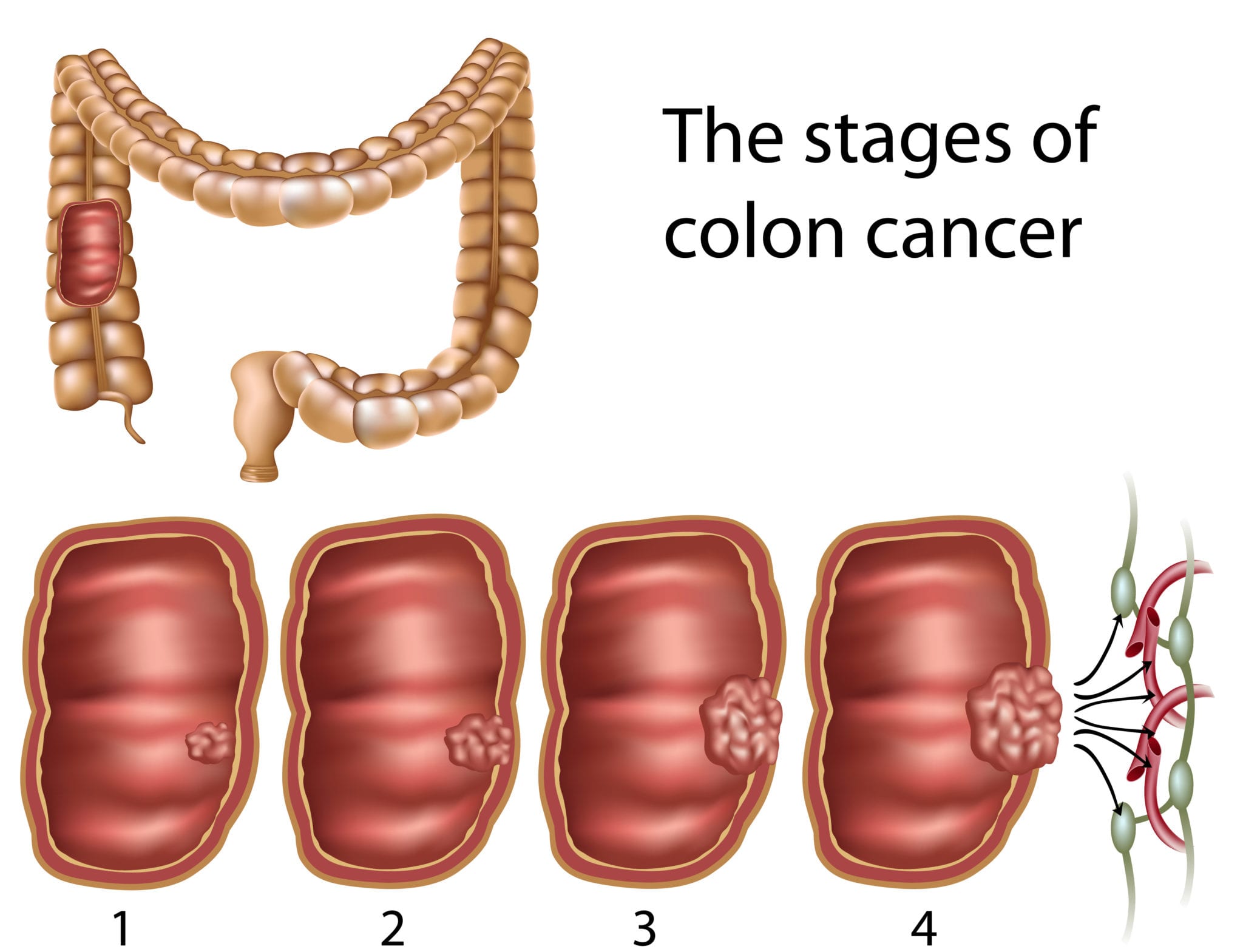
Stages 3 and 4 have grown to or through the muscular layers of the colon and spread to lymph nodes.
Lifestyle risk factors include:
- Overweight
- Lack of physical activity
- History of smoking (long-term smokers have a 30-50% greater risk)
- Heavy alcohol use
- Diet of red meat and processed meats
Related video: Why Meat is Linked to Colon Cancer

![]() Karen’s Fit Tip: If you haven’t had a checkup in a while, call your doctor this week and make an appointment. Know your risk. Since these silent killers are linked to the way you live, reduce your risk by changing your lifestyle. Eat healthy, stop smoking, limit alcohol, exercise, manage stress, and get sound sleep.
Karen’s Fit Tip: If you haven’t had a checkup in a while, call your doctor this week and make an appointment. Know your risk. Since these silent killers are linked to the way you live, reduce your risk by changing your lifestyle. Eat healthy, stop smoking, limit alcohol, exercise, manage stress, and get sound sleep.
IMPORTANT NOTE: If you have risk factors, a diagnosed condition, or a family history of certain diseases, talk to your physician. The types of tests, when you start testing, and how often you test may differ from the standard recommendations.