February is American Heart Month and marks the time to raise awareness about heart disease and how you can prevent it. Nearly 650,000 Americans die of heart disease every year — that’s one in every four deaths. Here’s why winter is prime heart attack season.

Flu Season and Heart Attacks — What’s the Connection?
Stress and inflammation caused by the flu are the same culprits that cause heart attacks. Heart attacks are six times more likely to occur 7 days after a flu diagnosis. Risk increases slightly if you’re over 65.
HEART ATTACK SEASON Typically flu season, thus heart attack season, falls between the start of fall and the end of spring. Historically, flu activity has peaked between the months of October and February, but tapers off by April. If you have a heart condition, it is critical to get your annual flu vaccine.
STRESS When you have the flu, the body is under a lot of stress. The heart has to work harder to pump blood through the lungs (which are inflamed from the viral infection), thus increasing the stress placed on the heart.
INFLAMMATION Flu can cause inflammation of the heart, brain, muscle tissues, and vital organs which can ultimately result in multiple organ failure.
 Inflammation can cause the plaque inside blood vessels to crack, rupture, and dislodge which results in a blockage within an artery.
Inflammation can cause the plaque inside blood vessels to crack, rupture, and dislodge which results in a blockage within an artery.- Oxygen levels and blood pressure can drop leading to an increased risk of forming blood clots in the blood vessels that feed the heart.
- Myocarditis (inflammation and destruction of the heart muscle tissue) can be caused by the flu and lead to rapid heart failure.
Heart Attack Season: Three More Reasons Why Winter is Problematic
1. COLD AIR TEMPERATURES. There are 53% more heart attacks in winter. A 16-year Swedish study of more than 280,000 patients suggests that the number of heart attacks peak in winter and that air temperature is an external trigger.
- Cold hurts the heart. It increases blood pressure and clot formation. When it is cold outside, the blood vessels in your extremities (arms, hands, feet, and legs) constrict to decrease heat loss from your skin which will increase arterial pressure.
- The elderly are especially at risk because they have less body fat and a diminished ability to sense temperature.
- Wind, rain, and snow also steal body heat.
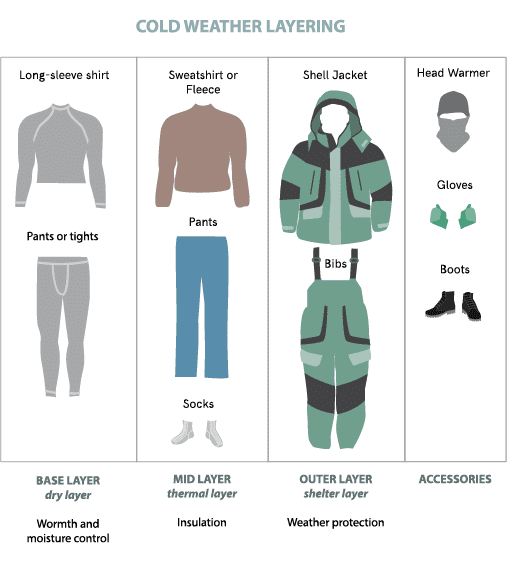
Dress in layers to trap heat.
2. OVEREXERTION IN THE COLD. Be wary of snow shoveling especially if you’re not a regular exerciser, have heart disease, or a chronic medical condition. Snow can be HEAVY. Shoveling is a vigorous activity and can put strain on your heart.

Cover your mouth and nose. Wearing a scarf or neck warmer allows the air to naturally get warmed before it enters your body, and thus, won’t be such a shock to your heart and lungs. This is especially critical for the elderly, people with heart disease risk factors, or have a cardiac history.
3.  MIXING ALCOHOL WITH COLD WEATHER. Drinking is especially dangerous when you’re out in the cold (e.g., at football games, skiing, walking at night, etc.)
MIXING ALCOHOL WITH COLD WEATHER. Drinking is especially dangerous when you’re out in the cold (e.g., at football games, skiing, walking at night, etc.)
- When it’s cold, your blood vessels constrict, but when you drink alcohol, your vessels dilate (widen) causing all your body heat to go to your skin and out to the environment.
- Your skin may feel warm and make you think your body is warming up, but actually, your core temperature is dropping which leads to hypothermia (when the body temperature drops below 95 degrees Fahrenheit).
- Drink water in the cold — not alcohol. Water is an insulator and retains body heat. Warm water is even better, so coffee and tea are good options when you’re cold.
Karen’s Fit Tip: Keep warm. Avoid big changes in temperature — especially when drinking. Wear suitable clothing (layers) when going from the warm indoors to the colder outdoors, even beyond winter time. In general, control chronic systemic inflammation with an anti-inflammatory lifestyle, i.e., a whole food, plant-based diet, limited intake of processed foods, regular exercise, no smoking, and fat loss (particularly abdominal fat) if carrying extra weight.





