When you walk or climb stairs, do you have… cramping, pain, aching, or tiredness in the muscles of your calves, thighs, buttocks, or hips? If so, you could have peripheral arterial disease (PAD), a narrowing of arteries (blockages) in your pelvis and legs.
Other symptoms can include:
- Leg numbness or weakness
- Cold legs or feet
- Sores on lower extremities that won’t heal
- Toenail color change
When PAD worsens, it’s typical to develop ‘exertional leg pain’, a symptom known as claudication. It occurs when you’re exerting yourself and feels like a muscle cramp. These symptoms usually go away after resting, but return when you walk again.
Do NOT try to “walk off the pain” or “tough it out”. Your limbs need to reoxygenate. Claudication does NOT go away if you continue to walk — it is only relieved by rest.
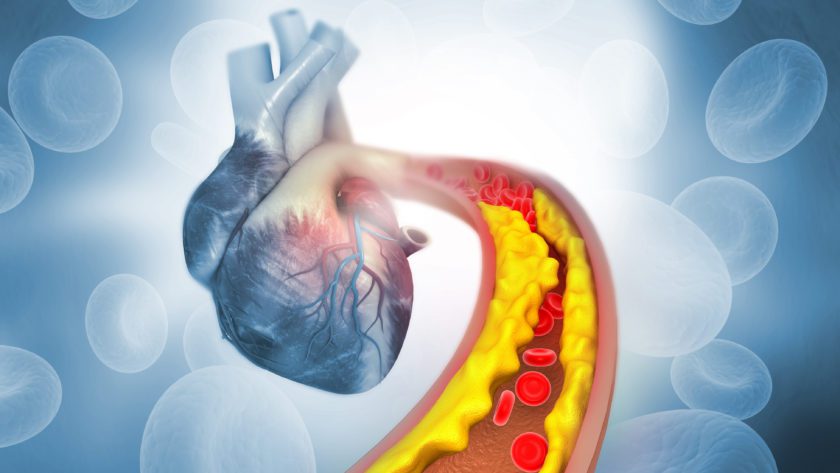
The pain is no different from ischemia (lack of oxygen) of your heart in that the delivery of oxygen does not meet the metabolic oxygen demand of working muscles.
What makes it worse when you’re walking is your blood has to move ‘upstream’ through narrowed arteries in your lower extremities to get back to your heart for more oxygen.
Intermittent ischemia of your skeletal muscles is uncomfortable, but not dangerous or life-threatening as is the case when your heart lacks oxygen, but as the disease progresses, it will be difficult to perform Activities of Daily Living (ADLs).
Then if the pain progresses to RESTING PAIN, there is a possibility of tissue death (gangrene), which is extremely serious.
BE AWARE: You could have PAD and not know it if you don’t walk long enough or far enough due to conditions like arthritis or pulmonary disease that limit your exercise tolerance.
If that’s the case, you won’t induce muscle ischemia and experience the subsequent ‘cramping’ in your lower extremities. Also, if you have diabetes, you could have neuropathies that deaden nerve endings in the legs, so you won’t feel any symptoms.
Risk Factors
- Smoking
- Diabetes
- Inactivity
- Hyperlipidemia (high cholesterol)
- Stroke
- Angina
- Hypertension (high blood pressure)
- Cardiovascular disease
- Advanced age
- Elevated levels of C-reactive protein (CRP) – a sign of systemic inflammation
Diagnosing PAD
A correct diagnosis is important because if you have PAD, you are at a higher risk for coronary heart disease (CHD), heart attack, stroke, and transient ischemic attack (TIA), commonly known as a “mini stroke”.
Once diagnosed, you may need to see a vascular specialist, a doctor who specializes in treating blood vessel diseases and conditions) for advanced PAD.
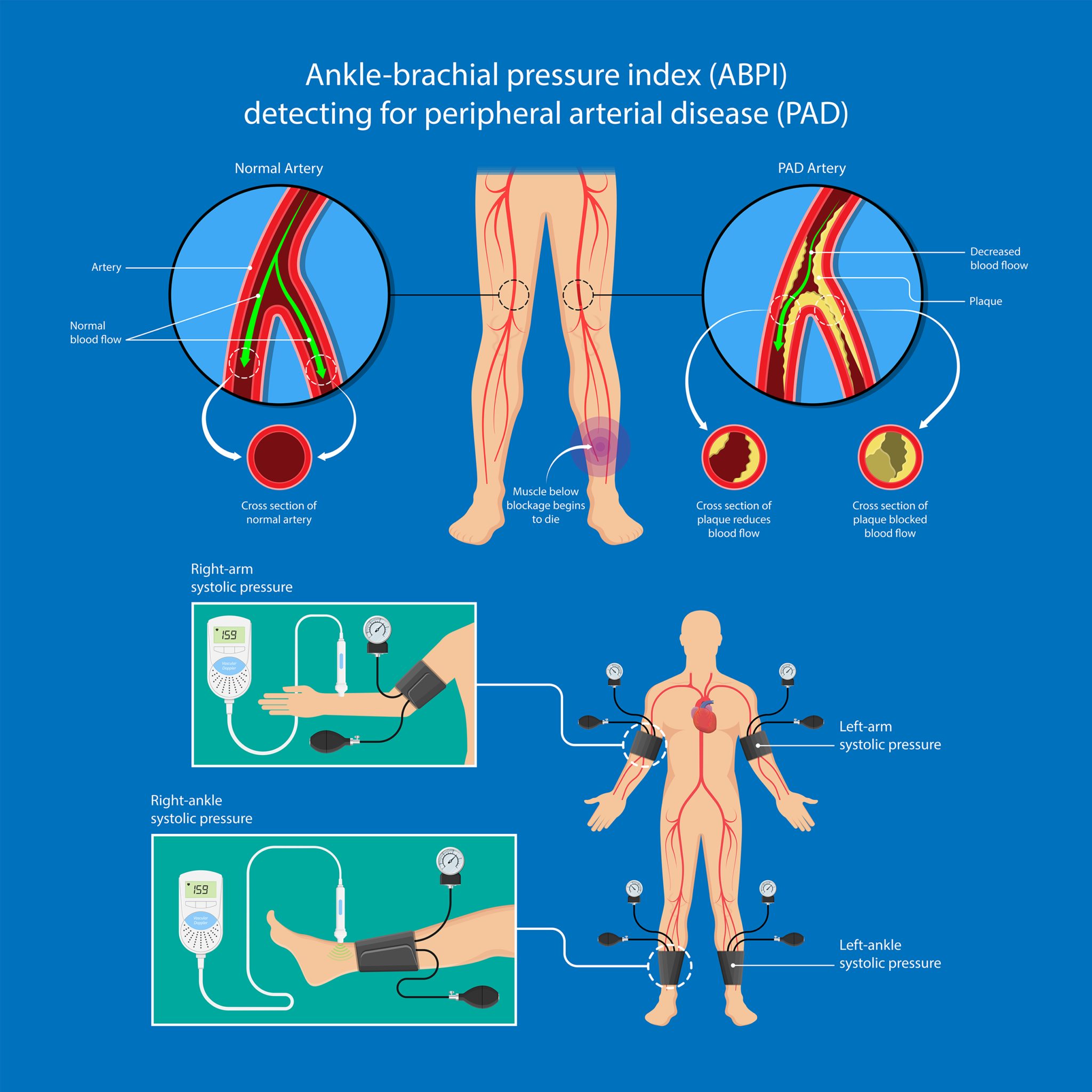
Your doctor will check blood flow (pulse) in the arteries in your legs or feet with a stethoscope and may also compare the blood pressure in your ankle with the pressure in your arm (Ankle-Brachial Index).
A Doppler ultrasound is often used to provide a good picture of blood flow in the major arteries and veins in the extremities.
What to Do if You Have PAD
- Quit smoking.
- Lower blood pressure to reduce risk of stroke, heart attack, heart failure, and kidney disease.
- Lower high cholesterol to delay or reverse buildup of arterial plaque.
- Lower blood glucose (sugar) levels if you have diabetes because high sugar levels can damage arteries.
- Exercise – Regular physical activity has been shown to reduce PAD symptoms.
![]() Karen’s Fit Tip: When exercising, increase intensity slowly and work BELOW your pain threshold (alternate walking with rest intervals).
Karen’s Fit Tip: When exercising, increase intensity slowly and work BELOW your pain threshold (alternate walking with rest intervals).
Also, talk to your doctor about the possibility of PAD if your exercise tolerance is low or you have diabetes. Be sure s/he is aware that you could have PAD but cannot induce muscle ischemia or recognize the symptoms.